Acute pain is a complex and multifaceted experience that serves as a critical warning signal for the body, indicating injury or illness. It typically lasts for a short duration, often less than three months, and is usually associated with a specific cause, such as surgery, trauma, or an underlying medical condition. Understanding the various types of acute pain is essential for effective diagnosis, treatment, and management. This guide will delve into the different types of acute pain, their characteristics, causes, and implications for treatment.
For a more comprehensive understanding of advanced acute pain relief strategies, you can refer to this comprehensive guide.
1. Somatic Pain
Definition
Somatic pain originates from the skin, muscles, bones, and joints. It is often described as sharp, aching, or throbbing and is usually well-localized, meaning that patients can pinpoint the exact location of the pain.
Characteristics
- Localization: Somatic pain is typically localized to a specific area of the body.
- Quality: Patients often describe it as sharp, dull, aching, or throbbing.
- Response to Movement: Somatic pain may worsen with movement or pressure on the affected area.
Causes
Somatic pain can arise from various sources, including:
- Injuries: Cuts, fractures, sprains, and strains.
- Surgical Procedures: Postoperative pain from incisions or tissue manipulation.
- Inflammation: Conditions such as tendonitis or bursitis.
Treatment
Management of somatic pain often involves:
- Non-Opioid Analgesics: Medications like acetaminophen and NSAIDs (e.g., ibuprofen, naproxen) are commonly used.
- Physical Therapy: Exercises and modalities such as heat or cold therapy can help alleviate pain and restore function.
- Rest and Rehabilitation: Allowing the affected area to heal while gradually increasing activity levels.
2. Visceral Pain
Definition
Visceral pain originates from internal organs and is often more diffuse and difficult to localize than somatic pain. It is typically described as deep, squeezing, or pressure-like.
Characteristics
- Diffuse Nature: Patients may have difficulty identifying the exact location of the pain.
- Quality: Often described as deep, aching, or cramping.
- Associated Symptoms: May be accompanied by autonomic symptoms such as nausea, vomiting, or changes in heart rate.
Causes
Visceral pain can result from:
- Organ Damage: Conditions such as appendicitis, pancreatitis, or cholecystitis.
- Inflammation: Inflammatory bowel disease or gastritis.
- Obstruction: Bowel obstruction or urinary tract obstruction.
Treatment
Management strategies for visceral pain may include:
- Medications: Opioids may be necessary for severe visceral pain, along with NSAIDs for inflammation.
- Surgical Intervention: In cases of organ damage or obstruction, surgical procedures may be required.
- Supportive Care: Hydration and nutritional support may be necessary, especially in cases of gastrointestinal distress.
3. Neuropathic Pain
Definition
Neuropathic pain arises from damage or dysfunction in the nervous system, including peripheral and central nervous systems. It is often described as burning, tingling, or shooting pain.
Characteristics
- Quality: Patients may describe the pain as burning, tingling, or electric shock-like.
- Location: Can be localized to a specific area or more widespread.
- Associated Symptoms: May include numbness, weakness, or hypersensitivity in the affected area.
Causes
Neuropathic pain can result from:
- Nerve Injury: Trauma, surgery, or compression of nerves.
- Diabetes: Diabetic neuropathy is a common cause of neuropathic pain.
- Infections: Conditions such as shingles (postherpetic neuralgia) can lead to neuropathic pain.
Treatment
Management of neuropathic pain often involves:
- Medications: Antidepressants (e.g., amitriptyline) and anticonvulsants (e.g., gabapentin, pregabalin) are commonly used.
- Topical Treatments: Lidocaine patches or capsaicin cream may provide localized relief.
- Interventional Procedures: Nerve blocks or spinal cord stimulation may be considered for severe cases.
4. Referred Pain
Definition
Referred pain is felt in a location different from the site of injury or damage. This phenomenon occurs due to the complex interplay of nerve pathways and the brain’s interpretation of pain signals.
Characteristics
- Location: Pain is perceived in an area distant from the actual source of the problem.
- Quality: The quality of referred pain can vary widely, often mimicking somatic or visceral pain.
- Confusion: Patients may be confused about the source of their pain, leading to diagnostic challenges.
Causes
Referred pain can occur due to:
- Visceral Organ Dysfunction: For example, heart pain may be felt in the left arm or jaw during a myocardial infarction.
- Musculoskeletal Issues: Pain from the spine may be referred to the legs or buttocks.
- Nerve Pathway Interactions: The overlapping of nerve pathways can lead to misinterpretation of pain signals.
Treatment
Management of referred pain focuses on addressing the underlying cause:
- Diagnosis: Accurate identification of the source of pain is crucial, often requiring imaging studies or diagnostic tests.
- Targeted Treatment: Treatment may involve medications, physical therapy, or surgical intervention depending on the underlying condition.
- Pain Management: Symptomatic relief through analgesics or other pain management strategies may be necessary.
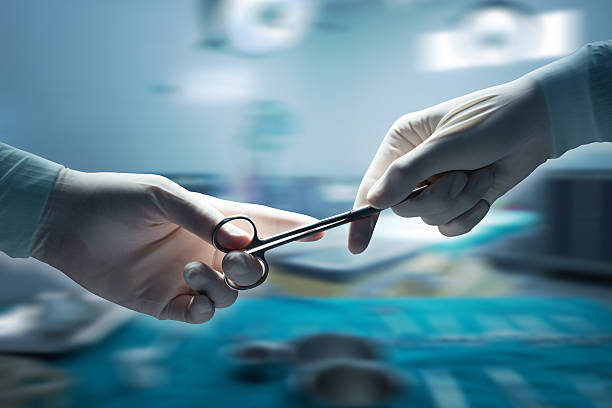
5. Acute Postoperative Pain
Definition
Acute postoperative pain is the pain experienced following surgical procedures. It is a normal part of the healing process and can vary in intensity based on the type of surgery and individual pain tolerance.
Characteristics
- Duration: Typically lasts for a few days to weeks, depending on the surgical procedure.
- Quality: Can range from mild discomfort to severe pain, often described as sharp or throbbing.
- Location: Localized to the surgical site but may also involve surrounding areas.
Causes
Postoperative pain can arise from:
- Tissue Trauma: Damage to skin, muscles, and nerves during surgery.
- Inflammation: The body’s natural response to surgical intervention.
- Complications: Infections or other postoperative complications can exacerbate pain.
Treatment
Management of acute postoperative pain often includes:
- Analgesics: A combination of opioids and non-opioid medications is commonly used.
- Regional Anesthesia: Techniques such as nerve blocks or epidurals may provide effective pain relief.
- Multimodal Approach: Combining different pain management strategies can enhance pain control and reduce opioid use.
6. Acute Injury Pain
Definition
Acute injury pain occurs as a direct result of sudden injuries, such as falls, accidents, or sports-related injuries. This type of pain is often immediate and can be intense.
Characteristics
- Onset: Pain typically begins suddenly at the time of injury.
- Quality: Often described as sharp, stabbing, or throbbing.
- Response to Movement: Pain may worsen with movement or pressure on the injured area.
Causes
Acute injury pain can result from:
- Trauma: Fractures, sprains, strains, or lacerations.
- Sports Injuries: Injuries sustained during physical activity, such as ligament tears or muscle pulls.
- Accidents: Injuries from falls, vehicle accidents, or other unexpected events.
Treatment
Management of acute injury pain may involve:
- RICE Method: Rest, Ice, Compression, and Elevation to reduce swelling and pain.
- Medications: NSAIDs or acetaminophen for pain relief.
- Physical Therapy: Rehabilitation exercises to restore function and strength.
7. Acute Inflammatory Pain
Definition
Acute inflammatory pain is associated with inflammation in response to injury or infection. It serves as a protective mechanism, signaling the body to heal.
Characteristics
- Symptoms: Often accompanied by redness, swelling, warmth, and tenderness in the affected area.
- Quality: Pain is typically described as throbbing or aching.
- Duration: Usually short-lived, resolving as the underlying inflammation subsides.
Causes
Acute inflammatory pain can arise from:
- Injury: Sprains, strains, or fractures leading to localized inflammation.
- Infections: Conditions such as cellulitis or abscesses.
- Autoimmune Responses: Conditions like acute arthritis or bursitis.
Treatment
Management of acute inflammatory pain often includes:
- Anti-Inflammatory Medications: NSAIDs or corticosteroids to reduce inflammation and pain.
- Rest and Ice: To minimize swelling and promote healing.
- Physical Therapy: To restore function and prevent stiffness.
Conclusion
Understanding the various types of acute pain is essential for effective diagnosis and treatment. Each type of pain has distinct characteristics, causes, and management strategies. By recognizing the differences, healthcare providers can tailor their interventions to meet the specific needs of patients, ultimately improving outcomes and enhancing the quality of care. Effective pain management not only alleviates discomfort but also plays a crucial role in the healing process, allowing individuals to return to their daily activities and improve their overall quality of life.
Also Read
- ► A Guide To Mastering The Art of Crafting Shareable Facebook Likes
- ► Ycloudx: Your trusted ERP system provider in Malaysia for 2025.
- ► Cash for Silver: Unlocking the Value of Your Silver Jewelry and Items in Delhi
- ► Stylish and Comfortable The Rise of SP5DER Hoodies
- ► Why Are Assless Chaps a Favorite in Biker and Fetish Fashion?
- ► Popular Courses to Study in UK After 12th for Indian Students
- ► The Influence of Comme des Garçons on Contemporary Fashion Culture
- ► How to Prepare for a VO2 Max Test: A Comprehensive Guide
- ► Best Engineering Assignment Help in New Zealand
- ► Solve Zone: Your Trusted Partner for Assignment Help
- ► Top PhD Thesis Writing Services in India – Solve Zone (2025)
- ► Top Materials Used by Office Workstation Manufacturers for Durability and Style
- ► Thailand Dedicated Server with AMD Ryzen 9 7900, 16GB RAM, 240GB SSD: Powerful Hosting
- ► Stüssy Clothing A Legacy of Streetwear and Cultural Influence
- ► Explore the Best Fruit Monster Vape Juice Flavors: A Flavorful Journey for Vapers